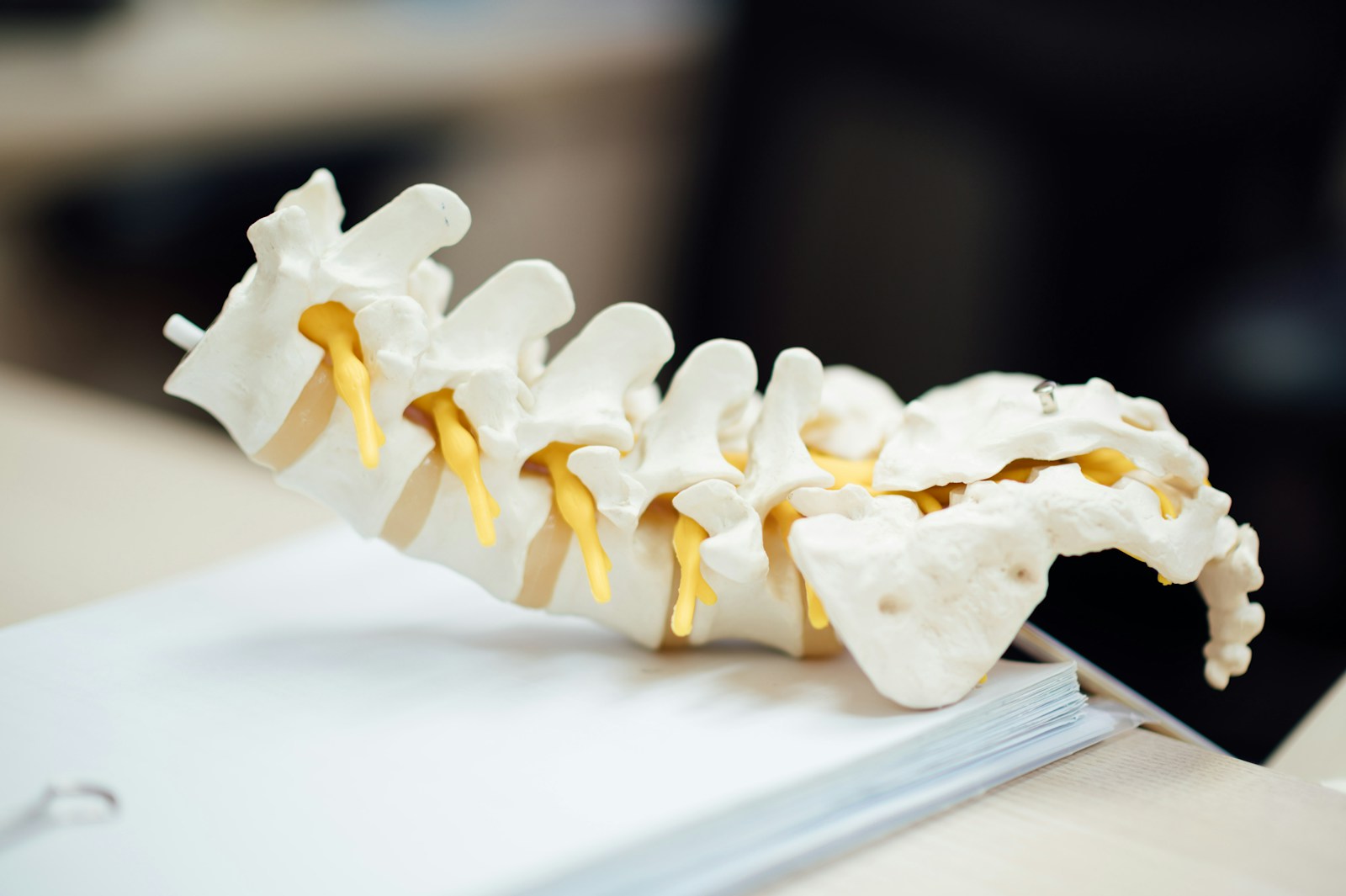
Foraminotomy is a neurosurgical procedure that enlarges the foramen to reduce spinal nerve compression. This advancement in spinal surgery relieves back and neck pain for patients. Its effectiveness and potential risks are areas of ongoing study in the medical field, contributing to the evolution of spinal surgery techniques.
Understanding Foraminotomy
In neurosurgery, a foraminotomy is a procedure that expands the foramen to alleviate spinal nerve compression and reduce back or neck pain. Despite misconceptions about its invasiveness and risk, advancements in medical technology have improved the surgery’s safety and postoperative outcomes. Insurance coverage for this procedure varies, but it’s often recognized as medically necessary for conditions like foraminal stenosis. It’s critical for patients to confirm coverage extent with their insurance providers.
Origins of Foraminotomy
The inception of foraminotomy is linked to early neurosurgery, with its purpose to alleviate spinal nerve compression. The evolution of neurosurgery led to the refinement of techniques, including foraminotomy. The inventors of this procedure aimed to provide relief without extensive surgery, recognizing the foraminal canal’s key role in spinal nerve function. Their goal was to create a method that allowed decompression without jeopardizing spinal stability. The advent of foraminotomy was a significant milestone in neurosurgery, offering a targeted approach to spinal treatment. This method focused on the precise area of nerve compression, limiting damage to adjacent tissues. It deviated from the invasive procedures of its time, setting the stage for modern minimally invasive spinal surgeries.
When Is Foraminotomy Needed?
Foraminotomy is needed when severe, persistent nerve compression symptoms like chronic pain, muscle weakness, or numbness fail to respond to conservative treatments. The surgical procedure, designed to widen the back opening where nerve roots exit the spinal canal, is considered after exhaustive monitoring and non-surgical treatments prove ineffective.
The foraminotomy decision isn’t solely based on clinical symptoms; cost factors significantly influence the process. These costs can fluctuate based on the surgeon’s experience, location, and case complexity.
Insurance coverage complexities add to the decision-making process. Not all policies cover foraminotomy, and coverage levels can differ. Understanding insurance terms and conditions, and discussing potential costs and coverage with the provider, is crucial. It’s essential to make an informed decision, considering both medical and financial aspects, before undergoing foraminotomy.
Foraminotomy Procedure Explained
The foraminotomy procedure, typically performed under general anesthesia, aims to alleviate nerve root pressure by enlarging the foramen – the spinal nerves’ exit point from the spinal canal. This surgical process starts with a small incision at the narrowed foramen site, followed by precise removal of compressing bone or tissue.
The cost analysis of foraminotomy considers the procedure’s complexity, which hinges on the extent of foramen narrowing and the number of vertebral levels affected. Additionally, it includes the professional fees of the surgical and anesthetic team, hospital stay, and post-operative care.
Recent advancements have significantly improved foraminotomy. The introduction of minimally invasive techniques and high-definition endoscopes has expedited recovery and enhanced patient outcomes. Furthermore, 3D imaging technologies have given surgeons a clearer view of spinal structures, allowing a more targeted approach during surgery. These advancements have refined the procedure and contributed to a more efficient cost structure.
Risks Associated With Foraminotomy
Foraminotomy, even with advancements, carries risks requiring patient-surgeon discussions. Understanding these risks—potential foraminotomy complications—is key to evaluating procedure success and post-surgical well-being.
- Infection Risks: Infections, either localized or systemic, could arise post-surgery. Antibiotics are a common preventative measure.
- Nerve Damage: Accidental damage to nerves during surgery may result in sensation loss or motor function impairment.
- Spinal Fluid Leak: Operating near the spinal cord presents a cerebrospinal fluid leak risk, potentially causing headaches and additional complications.
- Re-herniation: Herniated discs may reoccur, necessitating further surgery.
Preparing for a Foraminotomy
For foraminotomy preparation, crucial steps ensure surgical success and patient safety. The pre-surgery consultation’s importance is paramount, enabling health assessment, risk identification, and surgical approach determination. Required preoperative tests offer health insights, while dietary changes may optimize surgical readiness.
Pre-Surgery Consultation Importance
Pre-surgery consultations, especially for foraminotomy, have essential roles.
- Consultations mitigate consultation anxiety, a common issue where patients feel stressed, confused or afraid of upcoming procedures. Detailed explanations of the procedure, risks, and expectations help to ease these anxieties, resulting in improved patient outcomes.
- These consultations address the emotional readiness of patients. Mental preparedness for the surgery and recovery process is essential.
- These consultations allow patients to ask questions and express concerns, facilitating informed health decisions.
- Consultations also establish trust between patients and physicians, crucial for successful surgery and recovery.
Required Preoperative Tests
The pre-surgery preparation for a foraminotomy involves mandatory preoperative tests. These tests evaluate the patient’s overall health and surgical readiness. This process includes interpreting preoperative bloodwork, reviewing blood cell counts and chemistry for anomalies that could impact surgical outcomes. Addressing test anxiety is also crucial as it can distort results. Therefore, healthcare providers must apply anxiety management strategies to secure accurate findings and ensure a successful foraminotomy.
Dietary Adjustments Pre-Surgery
Before a foraminotomy, certain diet changes are needed for optimal health and improved surgical results. Nutrition’s role in health and recovery is key.
- Protein Increase: Necessary for tissue repair and immune function. Aim for lean protein like chicken, fish, or plant-based sources.
- Hydration: Maintains fluid balance, assists digestion, and keeps organs functioning. Adequate water intake is vital.
- Lower Sodium: To avoid hypertension and water retention, consume a low-sodium diet.
- Fruit and Vegetable Consumption: High in vitamins, minerals, and fiber, these foods support healing and immunity.
These diet modifications aid in successful surgery and quicker recovery.
The Day of the Surgery
On the foraminotomy day, essential sequences occur. Initial steps involve pre-surgery preparations: health evaluations, patient stabilization, and surgical team discussions. Then, the surgical procedure progresses systematically, showcasing precision and meticulousness in each step of this complex process.
Pre-Surgery Preparations
For successful foraminotomy surgery, follow these four preparation steps:
- Physical readiness: Maintain optimal health and fast as per surgeon’s instructions.
- Medication review: Consult your doctor about current medications, some may be stopped before surgery.
- Psychological readiness: Understand the procedure to reduce anxiety. Ask your surgeon any outstanding questions.
- Support system: Organize a trusted person’s presence for comfort and anxiety relief.
Each step enhances surgical results and comfort for the patient.
Surgery Procedure Steps
The foraminotomy procedure commences with general anesthesia administration, ensuring patient comfort. A surgical incision in the back grants access to the impacted region. Precision-guided instruments remove bone or tissue causing nerve compression. The task demands precision and stability to reduce risks like nerve damage, infection, or excessive bleeding. Post-surgery, patient experiences diverge; some feel immediate relief, others endure residual discomfort during healing. Regular follow-ups are paramount for monitoring recovery and managing complications. Thus, despite its complexity, foraminotomy effectively mitigates severe symptoms.
Post-Operative Care
After a Foraminotomy, post-operative care involves four key areas:
- Pain Management: This crucial aspect involves administering analgesics, NSAIDs, or opioids, depending on pain severity.
- Wound Care: Regular wound dressings, infection sign monitoring, and timely suture removal ensure a clean surgical site.
- Medication Adherence: To prevent infection, patients need to adhere to prescribed antibiotics and pain medications.
- Activity and Lifestyle Modifications: Patients should avoid strenuous activities post-Foraminotomy, and gradually resume activities under medical supervision for faster recovery.
Physical Therapy After Foraminotomy
Physical therapy post-Foraminotomy is crucial for patient recovery, focusing on spine rehabilitation and mobility improvement. This recovery phase enhances functional capacity and life quality post-surgery.
The therapy’s key aspect is posture correction, addressing spine misalignment, a contributor to nerve compression that Foraminotomy resolves. Therapy aims at posture correction for optimal spinal alignment, fostering recovery, and preventing nerve compression recurrence. Techniques employed encompass ergonomic adjustments, core muscle strength training, and education on correct sitting, standing, and lifting methods.
Mobility exercises are also prioritized in recovery. Designed to restore flexibility, minimize stiffness, and expand spine and muscle motion range, these exercises aid in reducing post-operative pain and swelling, enhancing circulation, and speeding up the healing process.
Expected Recovery Timeline
The foraminotomy recovery timeline typically consists of three stages: post-procedure, mid-recovery, and final recovery. Each stage includes specific milestones and treatments aiding in overall healing. A closer look at these stages clarifies expected recovery duration and progression, offering insight into the patient’s journey from surgery to full recovery.
Initial Post-Procedure Phase
Post-foraminotomy, the recovery timeline varies per patient, dictated by individual health and procedure complexity. Key recovery aspects include:
- Pain Management: Prescribed medication manages post-operative discomfort. Regular pain assessments refine medication plans for optimal relief.
- Emotional Support: Psychological health is crucial. Support from loved ones or counseling aids in managing recovery-related emotional stress.
- Physical Limitations: Patients should avoid strenuous activities post-surgery to prevent complications.
- Follow-up Appointments: Regular surgeon visits monitor progress and adjust recovery plans as needed.
Midway Healing Process
Around the four to six week mark post-foraminotomy, patients typically observe a decrease in pain and an increase in mobility due to body’s natural healing mechanisms and pain management strategies. Clinicians usually prescribe a mix of physical therapy and medications to assist recovery and reduce discomfort. The healing process also positively influences mental health as physical symptoms lessen. Nevertheless, healing timelines can fluctuate based on factors like overall health, surgery complexity, and adherence to post-operative care.
Final Recovery Stage
Post-foraminotomy full recovery, marking pain cessation and normal function resumption, typically occurs within three to six months. This timeline varies based on individual health factors and adherence to prescribed rehabilitation routines.
The final recovery stage encompasses four key milestones:
- Pain management: Employing effective strategies, such as medication and physical therapy, accelerates recovery and enhances quality of life.
- Lifestyle modifications: The adoption of healthy habits, including regular exercise, balanced nutrition, and strenuous activity avoidance, supports the healing process.
- Regular follow-ups: Consistent surgeon consultations monitor progress and promptly address complications.
- Return to normal activities: Gradual resumption of regular activities indicates successful recovery.
Each patient’s recovery timeline is unique, reflecting their individual circumstances and resilience.
Success Rates of Foraminotomy
Assessments of foraminotomy’s efficacy indicate high success rates, with many patients reporting substantial symptom relief post-procedure. The procedure’s success hinges on factors including surgeon expertise, spinal condition severity, and patient health.
Foraminotomy, a specialized procedure demanding skilled surgeons and advanced equipment, can be costly. However, its high success rates often validate the expense due to potential improvements in life quality and reduced long-term healthcare costs.
Insurance coverage for foraminotomy varies widely, making it essential for patients to comprehend their policy before proceeding. Coverage can range from majority to partial, sometimes necessitating high deductibles.
Alternatives to Foraminotomy
Foraminotomy alternatives offer symptomatic relief for spinal conditions and range from non-surgical to surgical methods.
- Physical Therapy: This non-surgical approach uses targeted exercises to strengthen spine-supporting muscles, reducing foramina pressure.
- Medication: Pain and inflammation can be managed using NSAIDs, steroids, or narcotics.
- Acupuncture: Supported by various studies, this non-surgical method stimulates specific body points to decrease pain and enhance mobility.
- Spinal Fusion Surgery: As a final option, this surgical procedure fuses vertebrae to limit movement and relieve nerve root pressure.
Frequently Asked Questions
Are There Any Specific Dietary Restrictions Before or After a Foraminotomy?
No specific dietary restrictions are necessary before or after a foraminotomy. However, pre-surgery hydration is vital. Post-surgery, increased caloric intake can support exercise and recovery, emphasizing the significance of balanced nutrition.
Is Foraminotomy Covered by Insurance?
Foraminotomy insurance coverage varies based on provider and plan. Typically, most insurers recognize it as a necessary procedure. Nevertheless, recovery time and costs may influence coverage extent. Consult your insurance provider for specific details.
How Does Foraminotomy Affect Overall Spinal Health in the Long Term?
Foraminotomy positively impacts long-term spinal health, reducing pain and increasing mobility. The recovery duration and therapy requirements differ among individuals. Consistent rehabilitation promotes beneficial health results over time.
What Is the Average Cost of a Foraminotomy Procedure?
The cost of a foraminotomy procedure, influenced by factors such as location and insurance coverage, averages between $15,000 and $50,000. Procedure alternatives and recovery time may impact the final expenditure.
Can a Foraminotomy Be Performed More Than Once on the Same Area?
Foraminotomy, depending on patient recovery and risk factors, can indeed be performed multiple times on the same area. Each situation, however, necessitates a unique evaluation.