Revision back surgery is a crucial intervention for patients experiencing unsatisfactory results from initial spinal procedures, persistent symptoms, or complications such as hardware failure. Determining the necessity for revision involves thorough diagnostic evaluations including advanced imaging techniques. These assessments guide the surgical team in selecting appropriate minimally invasive or decompression techniques tailored to address the underlying spinal issues. However, the complexity of such surgeries necessitates meticulous preoperative planning and coordinated postoperative care. What strategies do healthcare providers employ to optimize long-term outcomes and improve the quality of life for these patients?
Reasons for Revision Surgery
Revision back surgery is necessitated by various factors, including failed initial surgery outcomes, recurrent or persistent symptoms, hardware complications, and progressive spinal degeneration. A primary driver for revision surgery stems from unmet patient expectations post-initial surgery, which may arise due to continued or exacerbated pain, limited mobility, or neurological deficits. This necessitates a thorough preoperative evaluation in order to align patient expectations with realistic surgical outcomes.
Furthermore, recurrent symptoms may indicate incomplete decompression or stabilization during the initial procedure, necessitating a more extensive revision approach. Hardware complications, such as loosening, breakage, or malposition of instrumentation, can also prompt the need for revision surgery. These complications can lead to biomechanical instability or neural compression, further exacerbating patient discomfort and functional limitations.
Alternative therapies, including physiotherapy, pharmacotherapy, and minimally invasive procedures, are often explored prior to contemplating revision surgery. However, their effectiveness may vary, and persistent symptoms may ultimately require surgical intervention. Progressive spinal degeneration, characterized by conditions such as adjacent segment disease, can compromise the structural integrity of the spine, thereby prompting the need for revision surgery to restore stability and alleviate symptoms. In sum, a multifaceted approach that takes into account patient expectations, alternative therapies, and precise surgical indications is essential for successful revision back surgery outcomes.
Common Indications
Common indications for revision back surgery encompass a range of clinical scenarios including persistent postoperative pain, mechanical instability, and complications related to spinal hardware. Persistent postoperative pain is a significant concern, often attributed to failed back surgery syndrome (FBSS), where initial surgical interventions do not deliver the anticipated relief. Mechanical instability, manifesting as spondylolisthesis or vertebral slippage, necessitates revision to restore spinal alignment and function. Additionally, complications such as hardware failure, including screw loosening or rod breakage, demand prompt surgical correction to mitigate further morbidity.
Patient expectations play a pivotal role in the decision-making process for revision surgery. Unrealistic expectations can exacerbate dissatisfaction and impact psychological well-being. Aligning patient expectations with achievable surgical outcomes is essential. Psychological impacts, such as anxiety and depression, are also prevalent among patients considering revision surgery. These psychosocial factors can significantly influence both the perception of pain and the overall success of the surgical intervention.
Diagnostic Evaluations
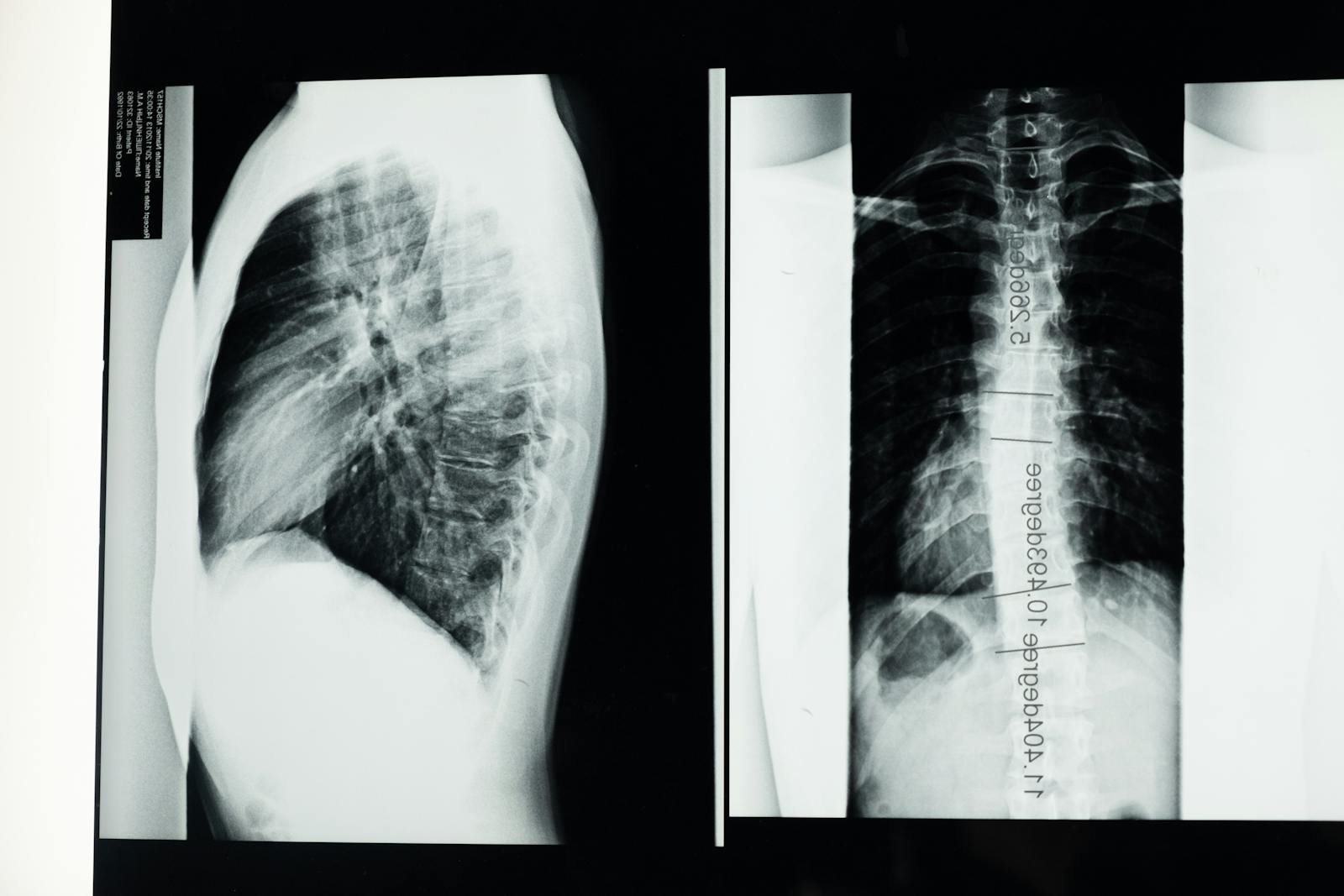
Diagnostic evaluations for revision back surgery are critical for identifying the underlying issues necessitating further intervention. Advanced imaging techniques such as MRI, CT scans, and X-rays are employed to provide detailed anatomical and pathological insights. Thorough preoperative assessment procedures, including patient history, physical examination, and functional status evaluation, guarantee a thorough surgical plan tailored to the individual’s specific condition.
Imaging Techniques Utilized
Effective evaluation of patients requiring revision back surgery often hinges on advanced imaging techniques that provide detailed anatomical and pathological insights. Cutting-edge imaging advancements such as magnetic resonance imaging (MRI), computed tomography (CT), and positron emission tomography (PET) have transformed the diagnostic landscape. These advanced modalities enable clinicians to pinpoint the precise etiology of postoperative complications, such as recurrent disc herniation, scar tissue formation, or hardware failure.
MRI remains the gold standard due to its superior soft tissue contrast, allowing for detailed visualization of spinal cord, nerve roots, and intervertebral discs. It is particularly adept at identifying epidural fibrosis and appraising adjacent segment degeneration. CT scans, with their high-resolution bone imaging, are indispensable for evaluating osseous structures and confirming hardware placement and integrity. When combined with myelography, CT can also delineate spinal canal compromise.
PET scans, although less commonly used, provide metabolic information that can differentiate between post-surgical scar tissue and recurrent neoplasm. These imaging techniques, often used in conjunction, offer a thorough diagnostic approach, facilitating precise surgical planning and optimizing patient outcomes. Employing these advanced imaging modalities is critical for the successful execution of revision back surgery.
Preoperative Assessment Procedures
In the context of preoperative assessment for revision back surgery, a thorough evaluation encompassing clinical history, physical examination, and laboratory tests is vital to identify underlying issues and guide the selection of appropriate surgical interventions. A meticulous clinical history should document previous surgeries, including the type, duration, and outcomes, as well as any complications. A physical examination aims to pinpoint neurological deficits, muscular strength, and range of motion.
Diagnostic laboratory tests, including complete blood count (CBC), metabolic panel, and coagulation profile, offer essential baseline data to confirm the patient’s physiological readiness for surgery. Additionally, specific biomarkers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can help identify underlying infections or inflammatory conditions.
Patient counseling is equally important, providing an opportunity to discuss surgical risks, benefits, and postoperative expectations. This dialogue fosters informed consent and optimizes psychological preparedness. A nutritional assessment evaluates dietary intake and identifies deficiencies that could impair wound healing and recovery. Malnutrition, often indicated by low serum albumin levels, necessitates dietary interventions or supplementation to enhance surgical outcomes. A tailored, evidence-based approach to revision back surgery, minimizing risks and improving prognoses, is achieved through comprehensive preoperative assessment procedures.
Surgical Techniques
Surgical techniques for revision back surgery encompass a range of advanced procedures tailored to address complications or failures from previous spinal surgeries. One vital approach is the use of minimally invasive techniques, which aim to reduce tissue disruption, minimize blood loss, and expedite recovery. These techniques often involve smaller incisions and the use of specialized instruments, such as endoscopes and tubular retractors, to access the affected spinal structures.
Instrumentation options play a pivotal role in the success of revision back surgeries. Surgeons may utilize a variety of fixation devices, including pedicle screws, rods, and interbody cages, to restore spinal stability and correct deformities. Advanced imaging technologies like intraoperative CT and fluoroscopy are employed to ensure precise placement of these instruments, thereby reducing the risk of further complications.
Additionally, the surgical approach may involve decompression procedures to alleviate nerve impingement, as well as fusion techniques to promote spinal stability. Autografts, allografts, and synthetic bone substitutes are often used to enhance the fusion process. By meticulously selecting and applying these surgical techniques, spine surgeons can greatly improve patient outcomes in revision back surgery, addressing both mechanical and neurological deficits.
Preoperative Planning
Preoperative planning for revision back surgery necessitates a thorough medical history review to identify prior surgical interventions, comorbidities, and potential risk factors. Diagnostic imaging tests, including MRI and CT scans, are essential for evaluating anatomical changes and pinpointing the source of persistent symptoms. Effective surgical team coordination ensures that all specialists are informed and prepared, optimizing intraoperative decision-making and postoperative outcomes.
Medical History Review
A thorough medical history review is vital in preoperative planning for revision back surgery, enabling the identification of potential risk factors and optimizing patient outcomes. This meticulous review commences with an exhaustive examination of the patient’s history, encompassing prior medical and surgical events, comorbidities, and any previous interventions. Understanding the patient’s surgical records is essential as it provides insights into prior procedures, the techniques employed, and the occurrence of any complications.
The clinician must evaluate the chronology and specifics of previous surgeries, including the type of surgical approach, the levels of the spine involved, and the nature of instrumentation used. This information is pivotal in discerning patterns such as recurrent infections, failed fusions, or persistent pain syndromes. Additionally, a detailed medical history review should include an assessment of systemic conditions like diabetes mellitus, osteoporosis, or cardiovascular diseases that may influence surgical risk and recovery.
Concurrent medications, including anticoagulants and immunosuppressants, should be meticulously documented to anticipate perioperative management. The history of any allergies, particularly to anesthesia or surgical implants, must also be recorded. This thorough approach ensures a tailored surgical plan, minimizing perioperative complications and enhancing the likelihood of a successful outcome in revision back surgery.
Diagnostic Imaging Tests
Thorough diagnostic imaging tests are indispensable in the preoperative planning for revision back surgery, providing critical insights into anatomical structures, existing pathologies, and previous surgical alterations. Advanced imaging modalities, including MRI, CT, and X-rays, play pivotal roles in accurately delineating the spine’s intricate anatomy. MRI, particularly with contrast agents, is highly effective in identifying soft tissue abnormalities, scar tissue, and recurrent disc herniations. Contrast agents enhance the visibility of vascular structures and inflammatory processes, offering a thorough view of potential complications or issues.
The advent of radiological advancements has greatly improved the precision of preoperative evaluations. High-resolution CT scans, for example, are invaluable for evaluating osseous structures and detecting hardware complications, such as screw loosening or fracture. These scans can be further enhanced with three-dimensional reconstructions, facilitating a more detailed surgical plan. Dynamic X-rays, including flexion-extension views, are crucial for evaluating spinal instability, which may not be apparent in static images.
Incorporating these sophisticated imaging techniques ensures a meticulous and individualized surgical approach. By leveraging these technologies, surgeons can mitigate risks, anticipate challenges, and improve the overall success rates of revision back surgeries. Accurate imaging thus forms the cornerstone of effective preoperative planning in this complex surgical domain.
Surgical Team Coordination
Effective surgical team coordination is paramount in preoperative planning for revision back surgery, ensuring that every team member is aligned on the procedural goals, potential challenges, and individualized patient considerations. Central to this coordination is robust team communication, which facilitates the dissemination of critical information regarding the patient’s medical history, prior surgical interventions, and current diagnostic imaging findings.
Role assignments must be clearly delineated to optimize workflow efficiency and minimize intraoperative complications. The lead surgeon is responsible for outlining the surgical strategy, including the identification of anatomical landmarks and potential pitfalls encountered in previous surgeries. Anesthesiologists must be apprised of specific patient requirements to tailor anesthesia protocols effectively, considering factors such as previous adverse reactions or comorbid conditions.
Nursing staff and surgical technologists play critical roles in ensuring the availability and sterility of specialized instruments required for the revision procedure. Coordination meetings, often involving multidisciplinary team discussions, are essential to preemptively address any potential intraoperative challenges and align on contingency plans. This methodical approach fosters a cohesive operative environment, augmenting the likelihood of successful surgical outcomes and swift patient recovery.
Risks and Complications
In revision back surgery, patients face a higher incidence of risks and complications due to the complexities involved in reoperating on previously altered anatomical structures. One significant concern is the heightened infection risks. Scar tissue from prior surgeries can obscure normal anatomical landmarks and impede the immune system’s ability to effectively combat pathogens. This necessitates meticulous aseptic techniques and potentially prolonged antibiotic prophylaxis to mitigate infection risks.
Formation of scar tissue, or fibrosis, presents another challenge. Scar tissue can adhere to neural structures, complicating dissection and increasing the risk of neural injury. Adhesions may also lead to impaired wound healing and chronic pain syndromes postoperatively. Additionally, the presence of extensive scar tissue can hinder the surgeon’s ability to achieve the best hardware placement, which is essential for spinal stability.
Other complications include dural tears, which can lead to cerebrospinal fluid leaks, and increased blood loss due to altered vascular anatomy. The risk of adjacent segment disease also escalates, as altered biomechanics from prior surgeries place additional stress on neighboring spinal segments. Therefore, thorough preoperative planning and advanced surgical techniques are imperative to mitigate these risks and improve patient outcomes in revision back surgery.
Recovery Process
The recovery process following revision back surgery necessitates a thorough approach that includes meticulous post-surgery care and adherence to physical therapy guidelines. Evidence suggests that tailored post-surgical care, encompassing wound management and pain control, greatly reduces the risk of complications. Concurrently, structured physical therapy protocols are essential for restoring functional mobility and promoting excellent healing outcomes.
Post-Surgery Care Tips
Successful recovery from revision back surgery necessitates adherence to a structured and evidence-based post-operative care regimen. A critical aspect of this regimen involves specific diet recommendations designed to facilitate tissue repair and reduce inflammation. Adequate protein intake, ranging from 1.2 to 2.0 grams per kilogram of body weight, is essential for muscle repair and collagen synthesis. Omega-3 fatty acids, found in fish oil and flaxseeds, exhibit anti-inflammatory properties that may expedite healing. Additionally, a well-balanced intake of vitamins and minerals, particularly vitamin C and zinc, is imperative for optimal immune function and wound healing.
Another cornerstone of post-surgery care is maintaining excellent sleep hygiene to enhance recovery. Sleep plays a significant role in regenerative processes, including the secretion of growth hormones and modulation of the immune response. Patients are advised to establish a consistent sleep schedule, ensuring 7-9 hours of quality sleep per night. The sleep environment should be conducive to rest, with minimal light and noise interference. Utilizing ergonomic pillows and mattresses can alleviate spinal stress, thereby supporting recovery. Adopting these evidence-based practices in diet and sleep hygiene can significantly improve post-operative outcomes for individuals undergoing revision back surgery.
Physical Therapy Guidelines
Adherence to a structured physical therapy regimen is crucial for maximizing functional outcomes and promoting thorough recovery following revision back surgery. The cornerstone of this regimen includes muscle strengthening and mobility exercises, which are essential for restoring spinal stability and enhancing functional capacity.
Initially, the focus is on gentle mobility exercises to prevent stiffness and maintain proper alignment. Passive range-of-motion exercises, facilitated by a physical therapist, help preserve flexibility without exerting undue stress on the surgical site. As healing progresses, active mobility exercises are introduced to improve dynamic control and neuromuscular coordination.
Muscle strengthening exercises play a pivotal role in the rehabilitation process. Core stabilization exercises target the lumbar and abdominal musculature to support the spine, reduce pain, and prevent recurrent injury. Progressive resistance training, incorporating isometric and isotonic contractions, is utilized to enhance the strength and endurance of paraspinal muscles and other supporting structures.
Evidence-based protocols recommend a gradual increase in exercise intensity and complexity, tailored to the patient’s tolerance and recovery milestones. Regular assessments by a physical therapist ensure that the regimen is effectively addressing the patient’s specific needs and facilitating excellent recovery. Compliance with these guidelines is essential to achieving long-term functional improvements and preventing complications post-revision surgery.
Pain Management
Effective pain management following revision back surgery often requires a holistic approach, incorporating pharmacologic interventions, physical therapy, and sometimes interventional techniques to address both acute postoperative pain and chronic pain syndromes. Among these interventional techniques, nerve blocks and spinal injections play a pivotal role. Nerve blocks, which involve the injection of anesthetic agents near specific nerves, can provide targeted pain relief by interrupting pain signal transmission. This method is particularly beneficial for patients experiencing nerve-related pain, which is common after back surgery.
Spinal injections, including epidural steroid injections and facet joint injections, are another cornerstone of pain management. These injections deliver corticosteroids and anesthetics directly into the epidural space or facet joints, reducing inflammation and providing significant analgesic effects. The efficacy of these interventions is supported by multiple clinical studies demonstrating their ability to alleviate pain and improve functional outcomes in postoperative patients.
Pharmacologic management typically involves a combination of opioid and non-opioid analgesics, such as NSAIDs and acetaminophen, to manage acute pain effectively. Adjunctive medications, such as muscle relaxants and anticonvulsants, may also be prescribed to address specific pain components. This integrated approach ensures effective pain control, facilitating a smoother recovery process.

Physical Therapy
Following revision back surgery, physical therapy plays an integral role in the rehabilitation process by enhancing functional mobility, reducing postoperative complications, and aiding in pain management. The structured implementation of exercise routines tailored to the patient’s specific needs is paramount. These routines generally begin with low-impact activities aimed at restoring range of motion and gradually progress to more demanding exercises that focus on strength, stability, and endurance.
Utilization of therapy equipment such as resistance bands, stability balls, and balance boards can greatly enhance the rehabilitation process. These tools facilitate targeted muscle engagement and proprioceptive training, essential for rebuilding core strength and ensuring spinal stability. Evidence-based practices underscore the importance of early mobilization within the first 24–48 hours post-surgery to mitigate risks of deep vein thrombosis and pulmonary complications.
Additionally, specialized modalities such as aquatic therapy can provide a low-gravity environment to ease joint stress while promoting muscle activation. Manual therapy techniques, including soft tissue mobilization and joint manipulation, are also employed to alleviate pain and improve tissue flexibility. Consistent monitoring and adjustment of exercise routines, based on the patient’s progress and feedback, guarantee a balanced approach to recovery, optimizing surgical outcomes.
Long-Term Outcomes
Evaluating the extensive outcomes of revision back surgery requires a thorough assessment of functional recovery, pain levels, and overall quality of life post-rehabilitation. Long-term outcomes are typically measured through various parameters such as patient-reported outcome measures (PROMs), radiographic evaluations, and physical performance tests. Patient satisfaction is a critical metric, often correlated with reductions in chronic pain and improvements in mobility. Studies indicate that successful revision surgeries often lead to significant pain alleviation, enhancing patient satisfaction.
In terms of functional recovery, patients commonly experience an increase in physical capabilities and a reduction in disability. Enhanced spinal stability and alignment, verified through radiographic imaging, contribute to these improvements. Additionally, lifestyle changes play a pivotal role in sustaining long-term outcomes. Patients are often advised to engage in tailored physical therapy programs and adopt ergonomic practices in daily activities, which further promote spinal health and prevent recurrence of issues.
Quality of life assessments post-revision surgery reveal marked improvements, particularly in social and occupational domains. Patients often report a higher degree of participation in daily activities and a return to work, underlining the efficacy of the procedure. Hence, thorough post-operative care and adherence to lifestyle modifications are essential for optimizing long-term outcomes in revision back surgery.
Patient Success Stories
Remarkably, the narratives of patients who have undergone revision back surgery provide compelling evidence of the procedure’s efficacy in restoring functionality and improving quality of life. Case studies reveal that many individuals experience substantial pain reduction and increased mobility post-surgery, underscoring the technical precision and expertise involved in these complex procedures. For example, a longitudinal study demonstrated that patients reported a 60% improvement in pain scores and a 50% enhancement in daily functional capabilities six months post-revision surgery.
Moreover, the emotional resilience exhibited by these patients is remarkable. The psychological burden of chronic pain and repeated surgeries often necessitates a robust mental fortitude. Recurring themes in patient testimonials highlight the importance of a supportive community, including family, friends, and healthcare providers, in facilitating recovery. This network not only aids in physical rehabilitation but also bolsters emotional well-being.
Additionally, advancements in surgical techniques and postoperative care have contributed significantly to these positive outcomes. Minimally invasive methods and personalized rehabilitation programs tailored to individual needs have been pivotal. Collectively, these factors demonstrate that revision back surgery, when executed with meticulous care, can offer renewed hope and greatly improved life quality.
Frequently Asked Questions
What Are the Costs Associated With Revision Back Surgery?
The costs associated with revision back surgery include hospital fees, which encompass operating room charges, anesthesia, and postoperative care. Insurance coverage greatly impacts out-of-pocket expenses, varying based on the patient’s specific policy and network agreements.
How Do I Choose the Right Surgeon for Revision Back Surgery?
To choose the right surgeon, evaluate their experience, reviewing their credentials and specialization. Additionally, assess patient testimonials for insights into outcomes and patient satisfaction, ensuring a well-suited decision for top-notch surgical expertise and care.
Can Lifestyle Changes Reduce the Need for Future Back Surgeries?
Implementing specific exercise routines and dietary modifications can greatly reduce the risk of future back surgeries. Evidence-based research demonstrates that strengthening core muscles and maintaining a balanced diet contribute to spinal health and overall well-being.
Are There Alternative Treatments to Revision Back Surgery?
Alternative treatments include physical therapy, which enhances musculoskeletal strength and flexibility, and pain management strategies, such as pharmacological interventions and nerve blocks, that can mitigate symptoms and improve patient outcomes without necessitating surgical intervention.
How Do I Mentally Prepare for Revision Back Surgery?
To mentally prepare, incorporate mindfulness techniques to manage stress and anxiety. Engage in support groups to share experiences and gain emotional support. These evidence-based strategies can enhance mental resilience and improve overall surgical outcomes.